Introduction
The spontaneous rupture of an OAA is a rare condition with a significant risk of life-threatening retroperitoneal hemorrhage. Over half of ruptured OAA among young women occur during pregnancy, mainly in the peripartum or postpartum periods. Despite its clinical significance, its true incidence remains unknown, as current knowledge is based on limited cases1,2.
The clinical presentation often mimics mild conditions or physiologic changes of peripartum status, potentially delaying diagnosis and leading to adverse outcomes. A high index of suspicion, along with early diagnosis and treatment, becomes essential to optimize the survival rates for both the patient and newborn in antepartum-related cases2.
In this context, we report and discuss the management of a postpartum patient with retroperitoneal hemorrhage following spontaneous rupture of a left ovarian artery (LOA) pseudoaneurysm. The patient was successfully treated with TAE, marking the 31st pregnancy-related case reported in English literature since 19633.
Case report
A 27-year-old Caucasian woman, gravida 3 para 2, was admitted at 38 weeks and 5 days of gestation for spontaneous labor. She delivered a male newborn weighing 2720 grams through uncomplicated vaginal delivery. Her medical records included Hashimoto’s thyroiditis, with no previous surgeries. The pregnancy was uneventful, aside from asymptomatic multiresistant Escherichia Coli bacteriuria at admission. Piperacillin-tazobactam was initiated in the immediate postpartum period.
On the 2nd postpartum day, the patient developed acute, severe left-sided flank pain, oliguria, and hypotension (70/50 mmHg). Physical examination revealed pallor, left-sided abdominal and lumbar pain, and abdominal distension unresponsive to analgesia.
Initial laboratory tests revealed a hemoglobin drop from 11 g/dL in late pregnancy to 9.3 g/dL, suggesting mild postpartum anemia. A renal-bladder ultrasound and an abdominal X-ray imaging (Figure 1) were performed, excluding urinary and intestinal complications. Persistent pain along with an episode of lipothymia prompted an urgent abdominopelvic contrast-enhanced CT-scan, revealing a 19 cm retroperitoneal hematoma in the left flank and iliac fossa (Figure 2). Additionally, a 7 mm pseudoaneurysm in the LOA was identified as the source of intermittent hemorrhage (Figure 3A).

Figure 1 Abdominal X-ray performed due to suspected intestinal obstruction, revealing displaced and distended intestinal loops with obscuration of the psoas muscle contour. These findings are nonspecific and have low sensitivity for detecting retroperitoneal hemorrhage, notably in low- to moderate-volume hematomas.
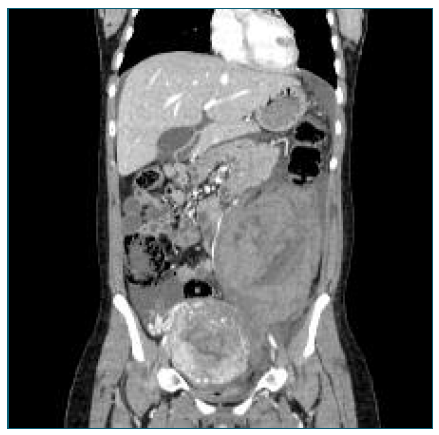
Figure 2 Abdominal-pelvic CT scan performed 2 days postpartum, showing a retroperitoneal hematoma measuring at least 12 × 13.4 × 19 cm (anteroposterior × transverse × longitudinal), localized in the left flank and iliac fossa. An enlarged uterus with a heterogeneous enhancement pattern results from normal postpartum changes.
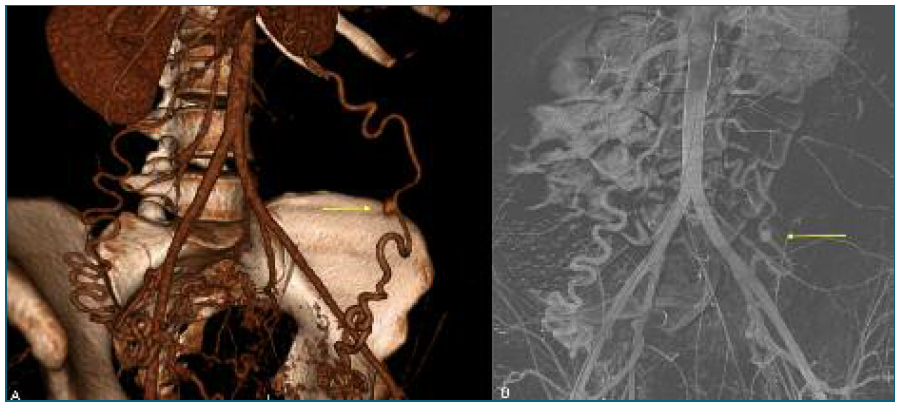
Figure 3 (A) Three-dimensional CT scan reconstruction showing a 7 mm saccular structure in the LOA, consistent with an ovarian artery pseudoaneurysm. No active bleeding was observed at the time of image acquisition, though intermittent hemorrhage was suspected; (B) Diagnostic angiography confirming the OAA in the LOA with active bleeding proximally to the pseudoaneurysm. The yellow arrows represent the OAA identified in both imaging diagnostic tools.
Hemoglobin dropped to 5.2 g/dL within a few hours, and the patient was transferred to the ICU to immediate resuscitation with 1 L crystalloid, 1 gram of tranexamic acid, and 3 units of red blood cells. After consultation with the vascular surgical team, the patient was taken to the Angio-Suite for urgent TAE. Approaching the common femoral artery, the LOA was selectively catheterized, and a diagnostic angiography confirmed the pseudoaneurysm (Figure 3B), with active bleeding at its proximal segment. Embolization of the proximal LOA was performed with 3.0- and 4.0-mm micro-coils. In attempting to microcatheterize the distal LOA, a new bleeding episode was identified, requiring additional embolization with thrombin and a 6.0-mm micro-coil (Figure 4A). Post-embolization angiography of the left hypogastric and common iliac arteries confirmed successful occlusion of LOA. (Figure 4B). Post-TAE, the patient was transfused an additional unit of erythrocytes, achieving a hemoglobin level of 8.5 g/dL. The patient had an uneventful recovery and was discharged within 5 days.
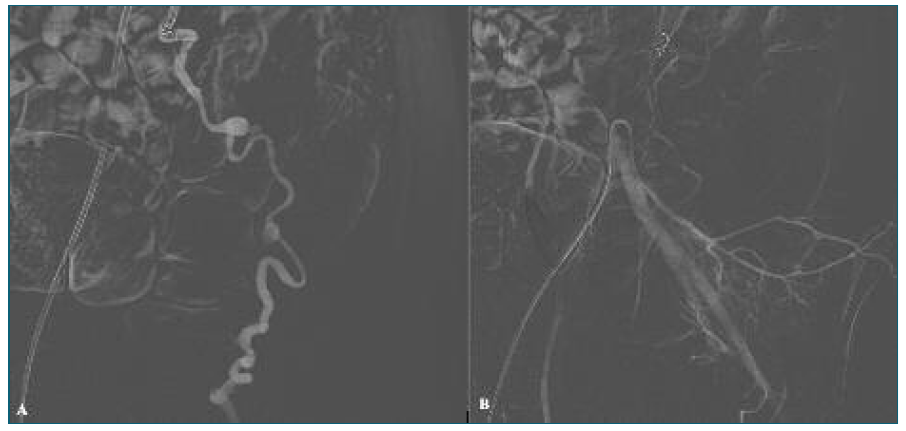
Figure 4 (A) Using a Cobra catheter via the common femoral artery, the proximal segment of the LOA was accessed and embolization with micro-coil was performed (MReye® coils, 3.0- and 4.0-mm). Due to contrast leakage after catheterization of the distal LOA, additional embolization with thrombin and a 6.0-mm micro-coil was performed. (B) Post-embolization control angiography through the left hypogastric and left common iliac arteries showed no evidence of active bleeding, confirming successful occlusion of the LOA.
By the 4th week postpartum, the patient presented a normal-ranged hemoglobin level (12.1 g/dL) with a normal physical examination. The patient underwent a multidisciplinary follow-up which included gynecology, internal medicine, genetics, and vascular surgery. At 6 months postpartum, a Next Generation Sequencing panel ruled out any causal variants of connective tissue disorders. Sequential CT-scans revealed retroperitoneal hematoma regression from 97 mm to 52 mm at 3 and 8 months postpartum, with complete resolution by 23 months (Figure 5). The patient remains under gynecological follow-up, being asymptomatic since post-TAE discharge.
Discussion
Acute retroperitoneal hemorrhage is a critical situation that may arise from various conditions, including iatrogenic (e.g abdominal trauma, surgical interventions) and spontaneous causes of arterial rupture, generally due to oncological or vascular disorders1. Arterial aneurysms and pseudoaneurysms are recognized causes, both distinguished by vessel wall integrity. Regarding pseudoaneurysms, the vessel’s wall becomes disrupted, potentially leading to the formation of periarterial hematomas and subsequent significant hemorrhage. Although vascular rupture has been documented in postmenopausal women, most cases occur during pregnancy or the peripartum period. The affected vessels often include the aorta, splenic, and renal arteries1,4. Since the first documented case of pregnancy-related OAA rupture in 1963, only 30 other cases, including ours, have been reported1-4. Pseudoaneurysms are even rarer than OAA, making this case of particular interest.
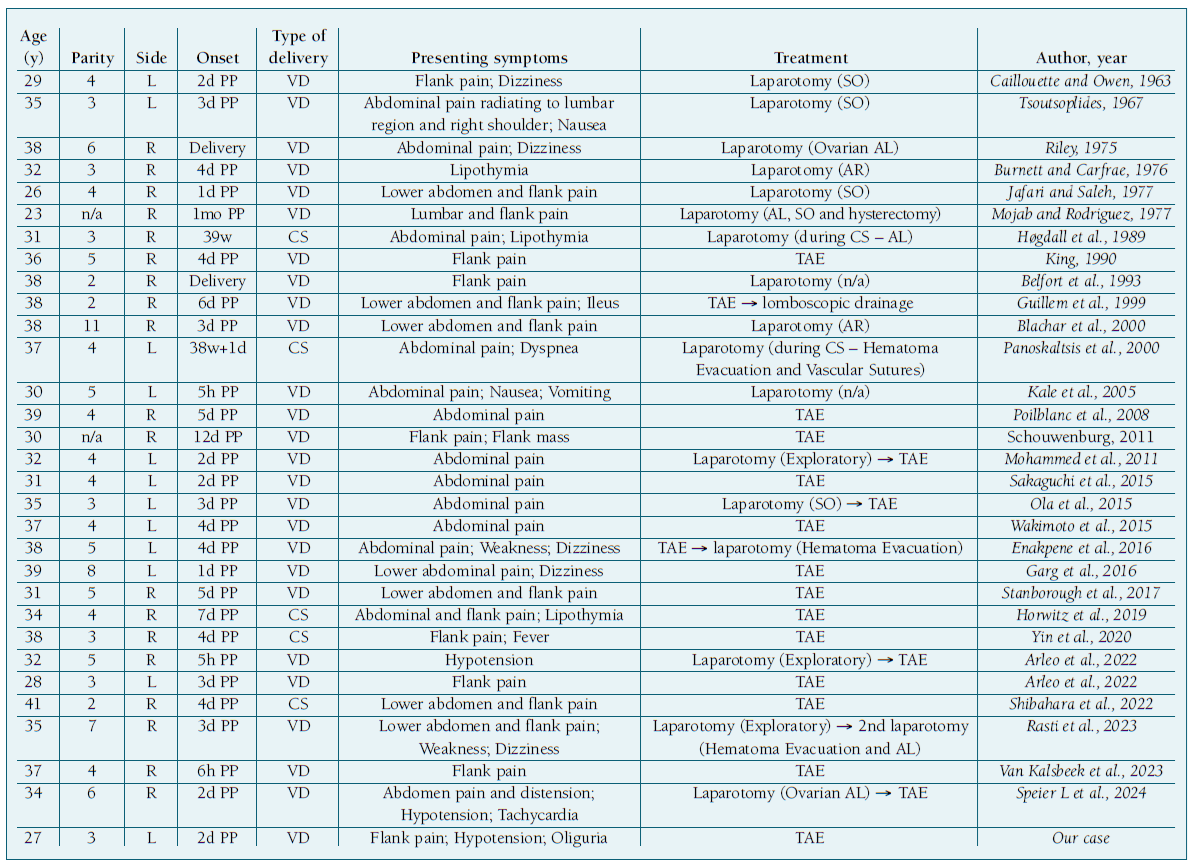
A literature review of pregnancy-related OAA rupture cases, summarized in Table I, shows a median patient’s age of 35 years (±4.4 years), with most being multiparous. Eighty-seven percent of cases occurred postpartum, with a mean onset of symptoms on the 4th day. Only 3 postpartum cases followed cesarean sections, and 61% of OAA ruptures were right-sided. This higher frequency of right OAA may be due to anatomical variations during pregnancy, as the uterus tends to deviate to this side5.
Table I Reported 31 cases of pregnancy-related spontaneous rupture of the ovarian artery1), (5-8),(14),(11-20.
Spontaneous peripartum hemorrhage from ruptured OAA mostly affects multiparous women, with pregnancy-related hemodynamic, anatomical, and hormonal changes playing a significant role in its pathophysiology6. Increased plasma volume and cardiac output, along with decreased vascular resistance, enhances utero-ovarian perfusion, predisposing ovarian vessels to vascular remodeling. Following uterine involution after childbirth, these vessels may become distorted as they regress, raising the risk of aneurysm formation and rupture4. Moreover, the increased circulatory sex steroids promote fragmentation of arterial elastic fibers and damage of the intimal layer, raising this risk with repeated pregnancies5-7. The link between delivery mode and OAA rupture remains unclear, though hormonal changes and expulsive efforts during delivery may explain its higher frequency among vaginal births5. Additional risk factors like uterine fibroids, hypertension, and connective tissue disorders (e.g. Marfan and Ehlers-Danlos Syndromes) were excluded in our case4. These findings emphasize the complexity of physiological changes in pregnancy. Therefore, the implementation of a preconception cardiovascular assessment and monitoring protocol could be beneficial in high-parity women. Currently, there are no established guidelines for managing asymptomatic OAAs, with recommendations based on limited reported cases8. However, secondary prevention strategies may include surgical correction before or during pregnancy, controlling blood pressure in cases of chronic or gestational hypertension, and promoting weight loss and smoking cessation9.
Typical presentation of ruptured OAA includes acute lower abdominal or flank pain, commonly seen in the reported cases (Table I). In situations of substantial retroperitoneal hemorrhage, clinical signs of hypovolemic shock may appear6. Therefore, the initial workup includes the evaluation of vital signs and physical examination, focusing on vaginal bleeding and abdominal findings. Due to its rarity, differential diagnosis barely considers the rupture of abdominal vessels. Their nonspecific symptoms may be easily mistaken with common postpartum conditions such as gastrointestinal and urinary tract disorders, delaying its recognition1),(4. Its challenging nature was exemplified in our reported case, requiring a systematical workup to rule out the more frequent causes before establishing the final diagnosis. An abdominal CT scan is generally performed for diagnosis at admission, although ultrasound is an alternative approach for pregnant women. Selective angiography, however, remains the gold standard for identifying the bleeding source4),(5.
There is no established treatment algorithm for OAA rupture cases, and both TAE and surgical interventions can be considered based on the patient’s hemodynamic stability, gestational age if applicable, and professional’s expertise4. TAE was performed in 61% of the reported cases, becoming the preferred approach in stable patients since its first use in 19901. Either treatment proved to be successful, with cessation of intraperitoneal bleeding in all patients. The average length of hospital stay was 8 and 14 days after TAE and surgery, respectively. In the literature, both laparotomy and TAE show similar mortality rates, although TAE is favored for its minimally invasive nature, resulting in reduced postoperative pain, fewer complications, and faster recovery4),(10. A wide range of embolic agents is available for TAE, including temporary (e.g. gelatin sponge particles, thrombin), and permanent agents (e.g. micro-coils, glue, N-butyl cyanoacrylate). Each embolic agent has distinct properties suited to specific clinical scenarios, and experienced vascular teams become essential to select the most appropriate one according to the patient’s comorbidities and desired outcome10. Nevertheless, surgical interventions including salpingo-oophorectomy, ovarian artery ligation, or aneurysm resection remain viable options in case of embolization failure, patient’s instability or limited access to interventional radiology4),(5.
Despite its benefits, selective TAE is not risk-free. Complications such as systemic thromboembolism, intraoperative arterial rupture, and non-target organ infarction, although infrequent, must be considered. Moreover, TAE does not allow hematoma evacuation, so close monitoring for pain and infection on residual hematomas is needed5),(7,10. Despite the need for hematoma evacuation due to persistent pain in 2/19 cases (10.5%), the only short-term complication post-TAE registered was a pulmonary embolism after 11 days2,5. Of the two antepartum cases registered, emergent cesarean sections were performed, and one neonatal death occurred11),(12. Most cases lacked long-term follow-up: one reported a subsequent pregnancy 3 months post-TAE, and those with follow-up up to one year showed no complications5,6,13-15. Our case stands out in the literature presenting more than 2 years of follow-up, without any complications recorded.
Regarding future fertility, current literature focuses only on non-target ovarian embolization following uterine TAE. Studies report a decrease on ovarian reserve in women over 40 years-old, but no impact was shown in younger ages16. Hence, concerns about ovarian ischemia or infarction post-TAE remain poorly understood and in need of primary research.
Conclusion
This case illustrates the need for prompt diagnosis of spontaneous OAA rupture. Although rare, especially for pseudoaneurysms, its presentation during pregnancy or the peripartum period may be masked by other common conditions, misleading the diagnosis. Awareness, particularly in high-parity women, is essential for timely recognition and treatment. While TAE appears effective, its short- and long-term effects, notably on fertility, need to be clarified. Furthermore, limited access to interventional radiology in smaller centers may affect optimal patient care. These challenges emphasize the need for ongoing research into OAA treatment and the establishment of standardized clinical management among affected patients.
Authors’ contributions
AB De Almeida: Substantial contributions to conception and design, data collection, analysis and interpretation of data; Article writing, reviewing and final editing. M Coroado: Contributions to data collection, critical review of article content; Final approval of the version to be published. CF Veiga: Critical review of article content; Final approval of the version to be published. CM Lourenço: Final approval of the version to be published. M Barreiro: Final approval of the version to be published.
















