Introduction
The physiological vaginal microflora primarily consists of Gram-positive bacilli from the Lactobacillus family. These organisms play a crucial role in maintaining a balanced environment by producing antimicrobial components such as hydrogen peroxide, bactericidal substances, and lactic acid. These components are responsible for lowering the vaginal pH (pH 3.5 - 4.5) and exerting toxic oxidative effects on anaerobic microorganisms, thereby avoiding the entry of potential infectious agents1. The dysregulation of this microbiota, due to decreased levels of Lactobacillus and consequent vaginal alkalinity, leads to a disruption of the environment, promoting dysbiosis such as Bacterial Vaginosis (BV), characterized by the replacement of Lactobacillus by anaerobic bacteria. The global prevalence of bacterial vaginosis in women of reproductive age in the general population is high, ranging from 23 to 29%, with racial disparities. According to geographical region, the prevalence also varies, as follows: Europe and Central Asia, 23%; East Asia and the Pacific, 24%; Latin America and the Caribbean, 24%; Middle East and North Africa, 25%; Sub-Saharan Africa, 25%; North America, 27%; South Asia, 29%. Since this is a prevalent disease, and also with concomitant high economic burden it is important to study the effectiveness of new therapeutic regimens2.
Diagnosis of this disease can be made based on Amsel criteria, which implies the presence of three of the following four signs: thin, homogeneous, non-irritating, white-grey vaginal discharge; vaginal pH > 4.5; fishy odor after application of 10% potassium hydroxide drops - positive amine test (whiff test); observation of clue cells upon fresh microscopic examination3. The Amsel criteria have been criticized because the assessment of the appearance of the discharge and the odour can be subjective and difficult to standardize, and therefore subject to misdiagnosis4. In addition, the use of the Amsel criteria also has low sensitivity when compared to the diagnosis of BV based on Gram staining or molecular tests. Diagnosis based on Gram stain has been widely accepted, especially in research studies. Gram-stained vaginal smears can also be interpreted repeatedly and by more than one evaluator, thus increasing the reliability of the diagnosis with this me-thod. The most widely used classification method based on gram staining is the Nugent index5.
Treatment of this condition typically involves antibiotics, such as topical and/or oral formulations of clindamycin or metronidazole1),(6-8.
Despite the wide use of antibiotics, there is a high recurrence rate, particularly within the first year following infection. It is believed that this may be due to the production and persistence of predominantly anaerobic biofilms, even after successful initial treatment7-9. Therefore, alternative therapeutic approaches, such as supplements, have been under investigation to enhance treatment efficacy and reduce the use of antibiotics, thus minimizing long-term resistance. Some studies have highlighted the benefits of Lactobacillus probiotics, lactic acid gel9, or antiseptics such as chlorhexidine or polyhexamethylene biguanide in the treatment of BV10.
More recently, there has been a growing interest regarding the role of ascorbic acid, as decreased levels of vitamin C have been observed in the vaginal fluid of women diagnosed with vaginitis11. Other studies have demonstrated that acidification of the environment, through the application of vaginal tablets containing 250 mg of ascorbic acid12,13, had a positive impact on normalizing initially abnormal vaginal microflora13. Therefore, it can be hypothesized that vitamin C may be beneficial in the treatment of BV.
Given the rationale outlined, the authors aim to investigate whether there is scientific evidence supporting the use of intravaginal vitamin C in the management of BV.
Methodology
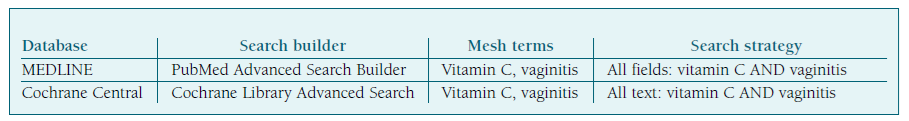
The authors conducted a systematic review by searching for indexed scientific publications in PubMed and Cochrane Central Library databases. The aforementioned research was conducted on October 30, 2023, and the related Medical Subject Headings (MeSH) terms used were “vitamin C” and “vaginitis”. No temporal filter was applied. Table I outlines the research process on the databases.
In order to address the aforementioned question, based on the PICO (Population, Intervention, Control, Outcome) acronym, articles written in English, Portuguese and Spanish, involving a population of women with an active diagnosis or recurrent history of BV-related vaginitis (Population), undergoing treatment or prophylaxis with vitamin C (Intervention) versus placebo or other first line/adjunctive/prophylactic measures used in BV (Control), were included to assess any potential efficacy of vitamin C in reducing symptoms/healing of BV (Outcome). Duplicated studies, articles of opinion, case reports or other reviews were excluded. Discrepancy between content of the article and the aim of this review was also considered an exclusion criterion.
All titles and abstracts were stored in the Google Sheets® platform and subsequently analyzed by two independent groups, each consisting of two authors of this study. After the initial screening, the same process was repeated for the full-text reading of the papers. Any discrepancies between the two groups during this process would be reviewed by the supervising author of the study, however, it was not necessary to reach this phase, as there was 100% agreement. This study enabled the authors to identify 264 articles, with five publications being included for discussion in this review. The steps of article selection are illustrated in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart in Figure 1.
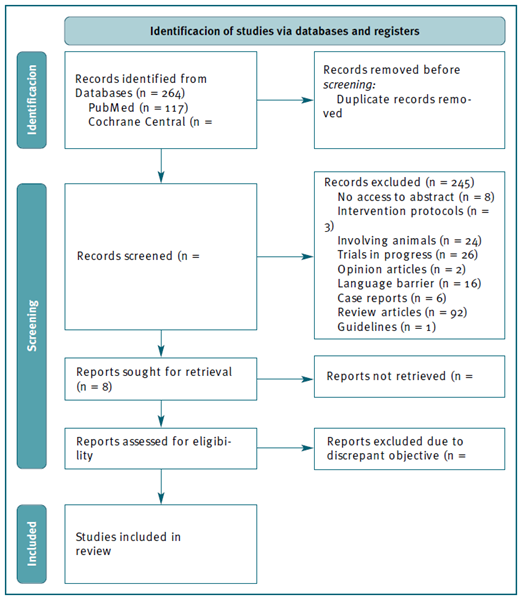
Figure 1 Flowchart according to PRISMA diagram regarding selection process of identified articles from databases. MEDLINE: Medical Literature Analysis and Retrieval System Online; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Quality assessment
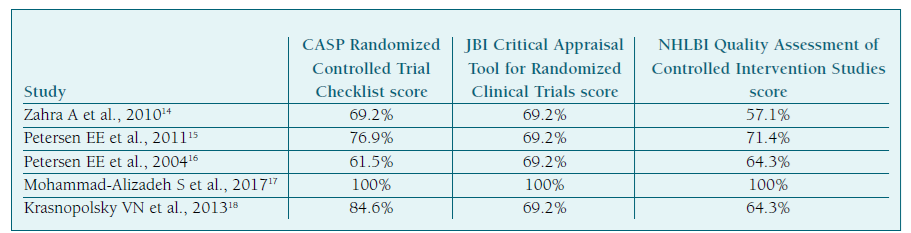
After the mentioned screening, the authors assessed the five included articles, described as randomized clinical trials, regarding the quality of their methodology. To do so, auxiliary tools for assessing the quality of randomized clinical trials were used, such as from Critical Appraisal Skills Programme, Joanna Briggs Institute or National Heart, Lung and Blood Institute. The compilation of quality appraisal scores for each study is presented in Table II. The authors established a score threshold of 50% or more for each article, across all tools, as the criteria for final inclusion in the results and discussion.
Results
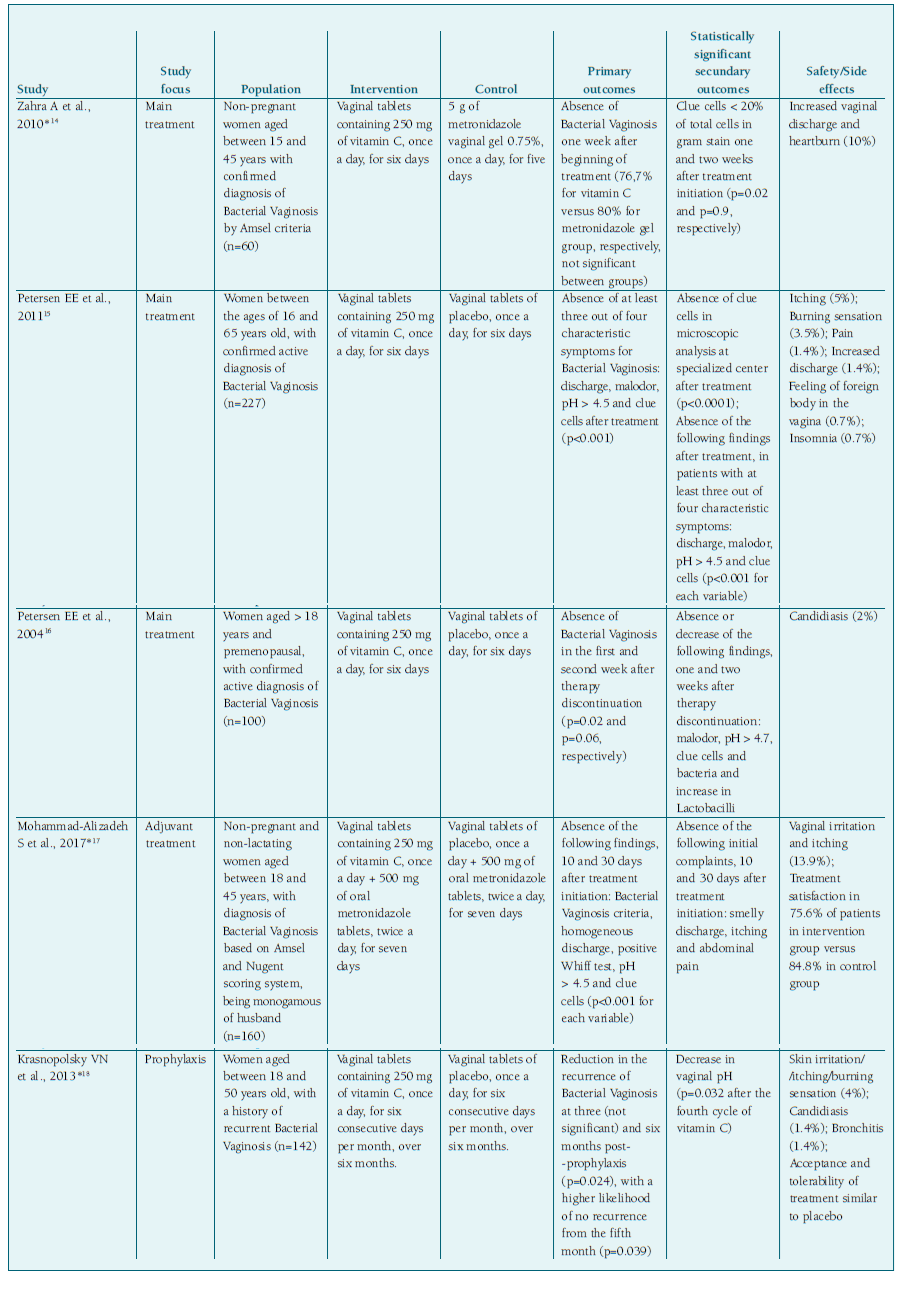
All five studies used intravaginal vitamin C at a dosage of 250 mg and studied premenopausal adult women with BV, with only two including adolescents14,15.
Regarding short-term treatment of BV, when compared with placebo, vaginal application of vitamin C resulted in higher cure rates after one to two weeks, as well as reduction in signs and symptoms such as malodor, pH and clue cells. However, statistical significance could not be proven for the improvement of vaginal itching15),(16. When compared to a first-line treatment like topical metronidazole, vitamin C did not demonstrate statistically significant superiority overall, except for the reduction of clue cells in the first week after treatment initiation. Despite the aforementioned, there was improvement in various parameters assessed with the use of vitamin C, including better BV cure rates when compared to metronidazole14.
In the only study comparing vitamin C to placebo as adjunct to antibiotic therapy, significantly better results were observed for vitamin C group regarding the absence of BV and improvement in the parameters of Amsel and Nugent criteria. There was also an improvement in initial complaints reported by patients, such as itching and abdominal pain, one month after the start of treatment17.
With respect to its prophylactic use, there was a reduction in recurrence of this condition after six months of prophylaxis, with a higher likelihood of no recurrence from the fifth month18.
Concerning safety of vitamin C, some adverse effects were evident in the studies analyzed, such as itching, burning sensation, irritation, candidiasis, or pain14-18.
Table III provides a compilation of the most important points regarding the publications included in this subsection.
Discussion
The results presented suggest a potential benefit of using 250 mg of intra-vaginal vitamin C in non-pregnant premenopausal women, as the main option or adjuvant treatment and prophylaxis of BV, as well as in controlling most of its characteristic symptoms and signs.
Regarding treatment of a BV episode, the application of intravaginal vitamin C, either as monotherapy or in conjunction with another treatment, once a day, for six to seven days seems to be clinically useful, with a good cure rate after one to two weeks, also supported at the microscopic level by a significant reduction in clue cells, which are highly characteristic of anaerobic presence, such as Gardnerella vaginalis. This effectiveness may be explained by the notable decrease in pH, consistent in the majority of the analyzed studies, and subsequent normalization of the previously alkaline vaginal environment, which promotes adversity to the anaerobic infectious agents, causative of BV19. It’s worth noting that the majority of studies compared vitamin C with placebo, with only one study comparing it with metronidazole. In the latter, similar efficacy was observed in both treatments, leading the authors to suggest that vitamin C may be a treatment option for BV17. However, further studies comparing vitamin C to other first-line therapeutic options in BV are needed to corroborate this assertion.
Concerning prophylaxis of BV, the prolonged use of 250 mg of vitamin C, for six consecutive days per month, after each menstruation, seems promising in reducing the recurrence of BV episodes, especially if prophylaxis is maintained for at least five months. Only the investigation carried out by Krasnopolsky VN et al. addressed the theme of vitamin C prophylaxis in BV18, so further studies need to be carried out in this area to corroborate the above. At the same time, it would be important to compare vitamin C with other prophylactic methods, such as probiotics20.
As for the safety of intra-vaginal vitamin C use, it can be used relatively safely, as there is a low frequency of adverse effects, with itching and burning sensation being the most frequent, and candidiasis occurring less frequently. In the study by Zahra et al, adverse effects were observed in 3 of 30 patients (10%) under treatment with vitamin C and in 4 of 30 patients (13.3%) under treatment with metronidazole, with no statistically significant difference observed17. In the study by Peterson et al, which compares the effectiveness of vitamin C with placebo, 2 patients out of 50 in the active group had candida superinfection as adverse effects and 2 patients out of 50 in the placebo group reported itching and cystitis, respectively, once again there were no significant differences between the groups regarding adverse effects16.However, it is important to note that the severity of symptoms was not observed, nor is there a direct causality between vitamin C intake and the occurrence of each of these symptoms, so further studies are needed in this regard.
This study, despite analyzing randomized double-blind clinical trials, has some limitations. Firstly, most of the database platforms encountered by the authors require payment for access, so the au-thors did not have the opportunity to conduct a more comprehensive search, as this study was not funded by partner entities. Secondly, regarding heterogeneity there are some points relatively population and study design that require discussion: the five studies included in this systematic review involved women of varying ages (15-65 years) and different diagnostic criteria for BV (Amsel and/or Nugent). The presence of comorbidities, such as sexually transmitted infections or other gynecological conditions, was not uniformly reported in the studies, which may have affected the response to treatment. In addition, participants’ marital status and sexual activity may influence exposure to risk factors for BV and the effectiveness of interventions. The studies also differed in terms of the type of intervention (vitamin C alone, metronidazole alone, vitamin C combined with metronidazole), the dose and duration of treatment. The control groups also varied, including placebo or metronidazole alone. The primary and secondary outcomes differed between the studies, making it difficult to directly compare the results. In addition, the follow up period varied throughout studies, which may have affected the assessment of the long-term effectiveness of the interventions. Overall, the heterogeneity of the studies included in this systematic review highlights the importance of considering the population and study design when interpreting the results of clinical trials of treatment of BV. Future studies should seek to standardize the diagnostic criteria, control groups and outcomes assessed in order to facilitate comparison between different interventions. In addition, it is important to consider the heterogeneity of the population, including factors such as age, comorbidities and sexual status, when planning and interpreting the results of clinical trials.
Additionally, this study is limited to only five publications, with the most recent one dating back to 2017, indicating the need for further research in this area. It should also be noted that the population analyzed in each of the articles did not include menopausal women, however, this aspect can be explained by the lack of data in the literature regarding ideal diagnostic criteria for BV in postmenopausal women21. Therefore, further studies are needed to address these limitations.
Author contributions
João Carlos Silveira - bibliographic research and selection, writing of the article. Ana Rita Fernandes - bibliographic research and selection, writing of the article. Catarina Pisco - bibliographic research and selection, writing of the article. Francisca Pinho Rocha - bibliographic research and selection, writing of the article. Vera Soares da Costa - supervision and critical review of the article.