IPV is a social and public health problem that affects women’s health in general. Global estimates of IPV indicate that about 30% of women experience some form of physical or sexual violence (Trabold et al., 2018). Data from the Centers for Disease Control and Prevention (CDC) National Intimate Partner and Sexual Violence Survey (NISVS) reported that about 1 in 4 women in the U.S. have experienced sexual violence, physical violence, and/or stalking by an intimate partner during their life, and that more than 43 million women have experienced psychological abuse by an intimate partner in their lifetime (CDC, 2019). In Portugal, IPV is considered the second most common crime against other people, representing 27.6% of all crimes (Sistema de Segurança Interna [SSI], 2017).
According to the literature, the experiences of women victims of IPV are associated with the acquisition of HIV/STIs (Durevall & Lindskog, 2015; Gibbs et al., 2018). Thus, there are several ways that IPV and HIV/STIs are related. For example, the increase in risky sexual behaviors between victims and the perpetrator of IPV (e.g., having unprotected sex, multiple sexual partners, and sexual intercourse under the influence of alcohol or drugs), the physiological and psychological consequences of violence that facilitate HIV transmission (e.g., being immunocompromised), having forced sex with an infected partner, and the inability of victims to negotiate condom use and other safer sexual practices (e.g., lack of control over sexual decision-making) (Gonzalez-Guarda et al., 2019). In addition, men who are abusive tend to engage in high-risk sexual behavior and are more likely to be HIV-positive and to have other STIs, thus increasing women’s risk of infection (Gibbs et al., 2018; Nguyen et al., 2017).
IPV histories are associated with a higher risk of acquiring HIV and other STIs, with higher rates of condom-free sex, and difficulties in interpersonal functioning (Braham et al., 2019). IPV has also been associated with less sexual assertiveness, less comfort with sexual negotiation, and greater sexual risk (Orchowski et al., 2020). Individuals who are less assertive with their sexual partners, when negotiating condom use, are less likely to insist on condom use, use condoms, or use condoms consistently (Braham et al., 2019). Indeed, systematic reviews of IPV suggest strong links with decreased condom use and decreased condom negotiation among women (Bergmann & Stockman, 2015).
Adverse childhood experiences are also public health problems that have a significant impact on future health and behaviors, such as sexual risk and IPV victimization (Willie et al., 2018). In 2019, globally, around 1 billion children were victims of violence (Lai et al., 2020). In the US, one in four children (25.6%) has been maltreated as a child and nearly one in five children (17.3%) witness parental IPV in their lifetime (Finkelhor et al., 2013). In recent years, there have been some investigations regarding sexual abuse that report prevalence rates of minors ranging from 5% to 18% (Gray & Rarick, 2018; Senn et al., 2017). In many cases, child sexual abuse has devastating consequences for the lives of those who suffer it, since it involves the disruption of the child’s behavior and emotions and sometimes seriously interferes with their development (Castro et al., 2019).
In a 30-year prospective study, Wilson and Widom (2008) found that individuals who were victims of childhood abuse were more likely to report early sexual contact (before age 15), engage in adult prostitution, and have an HIV positive test during adulthood than individuals who had not been abused. According to Miller’s (1999) pioneering paper, the relationship between child abuse and HIV risk behaviors can be explained by alcohol and drug use, sexual maladjustment (such as deficits in sexual risk recognition), psychopathology, and social networks of risk. Thus, it explains that abused women engage in risky sexual practices due to behaviors and beliefs about sexuality that they developed in response to abuse. In fact, there is empirical evidence linking each of these proposed mechanisms of childhood trauma to HIV risk behaviors (Weiss et al., 2019).
Following the explanatory analysis on the relationship between childhood trauma and HIV risk behaviors, the literature review suggests that childhood trauma may explain, at least in part, HIV risk behaviors in women victims of IPV (Weiss et al., 2019). Castro et al. (2019) report that previous studies have concluded that victims of childhood sexual abuse exhibit riskier sexual behaviors and are more likely to experience new episodes of sexual victimization during adolescence and early youth. Additionally, several studies found that people who have experienced an episode of childhood sexual abuse have an early onset of penetrative consensual sex (Gray & Rarick, 2018), more sexual partners, inconsistent condom use (Senn et al., 2017) or increased drug use in sexual relationships, and consequently are more vulnerable to having STIs (Castro et al., 2019).
According to the literature on female re-victimization, there is empirical evidence on the relationship between childhood abuse experiences and IPV in adulthood, both in retrospective and prospective studies (Widom et al., 2014). Most theoretical explanations for the relationship between child abuse and IPV emphasize that abused children are potentially limited in their psychological and social development, which conditions the selection of partners in adulthood, as this selection is oriented towards satisfy short-term psychological and social needs, which may have harmful consequences for women in the medium and/or long term (Herrero et al., 2018). In some cases, this selection of inappropriate intimate relationships can include potentially abusive male partners, which increases the likelihood of IPV (Herrero et al., 2018).
Intergenerational transmission theory of violence and social learning theory explain that IPV is higher among women who were abused in childhood or who witnessed parental violence (Bandura, 1977; Machisa et al., 2017). This research is supported by theoretical frameworks such as the intergenerational transmission theory of violence and social learning theory. The intergenerational transmission theory of violence suggests that IPV is passed from generation to generation, so that children who are abused and/or who have witnessed parental IPV are more likely to use and experience violence in later relationships (Egeland, 1993). Social learning theory explains also that children who witness or experience abusive caregiver behavior during childhood learn that aggression is an acceptable means of resolving conflict (O’Leary, 1988). As a result, women who are exposed to violence when children learn to be aggressive with their partners, or to be more tolerant of aggression from their intimate partners (Smith & Stover, 2016).
Previous studies (Weiss et al., 2019; Willie et al., 2018), which have assessed the relationship between traumatic childhood experiences and IPV, focus mainly on mental health leaving out sexual risk behaviors. Therefore, the present study aims to address this specific gap analyzing the contribution of IPV and childhood trauma to HIV risk behaviors, and to study differences between victims and non-victims, in order to intervene more effectively with this population, reducing their vulnerability.
Method
Participants
Data were collected from 141 women, from which 61 were battered women who attend victim support associations and shelter houses, among other victim support entities in the north of Portugal, and 80 non-victims collected from the general population of the same geographical area at public and private primary health care services. Participants were recruited from victim support associations and primary healthcare services in northern Portugal. Women victims of IPV were recruited from all the aforementioned support systems over approximately one year. These support systems provide psychosocial and legal support for victims as well as protective shelter. For inclusion in the study, participants must have reported being in a relationship for at least one year, 18 years of age or older, and able to speak and write Portuguese proficiently. To meet preliminary screening for the IPV group, women had to report at least one incident of aggression in the past year. The same inclusion criteria were used for the non-victims, except for the incident of aggression.
Procedures
Between November 2019 and July 2020, 61 women victims of IPV were invited to complete an interview for the current study if they were seeking psychological and legal assistance in the several victim support systems and had a documented incident of abuse from an intimate partner as defined by their responses to the Revised Conflict Tactics Scale 2 (CTS2) (see below). Eighty non-victims were collected from the general population and completed the same questionnaires (including the CTS2) lasting approximately 1 h. Study procedures were approved by the Institutional Review Board and Ethics Committee of victim support systems. All participants signed a written informed consent explaining the purpose of the research and that they have the right to withdraw at any time, with participation being voluntary and confidential. At an initial stage, the questionnaires were delivered in paper format, and at a later stage, they were made available in online format, through Google Forms, for security reasons related to the COVID pandemic. Measures employed in the present study are described below.
Measures
A structured interview was used to collect information on socio-demographic characteristics for women victims of IPV and non-victims (i.e., age, education, employment status, marital status, and number of children). The women were also asked about the relationship with the perpetrator, cohabitation with the perpetrator, and duration of victimization.
Intimate Partner Violence (IPV) severity - The CTS2 (Straus et al., 1996) were used to assess the severity of different types of IPV participants experienced. Although the CTS2 has two dimensions (perpetration and victimization), we only used the victimization items (39 items), leaving out the negotiation subscale (6 items). Therefore, in the present study we used a total of 33 items. Participants rated the frequency that each abusive act occurred during the past year with their dating partners. In the present study four subscales were used: physical violence with and without injury, sexual coercion and psychological aggression. The participants were asked to rate their experience on a 7-point Likert scale from 0 (this has never happened to me) to 6 (this has happened more than 20 times). Internal consistency reliability with coefficient alphas for the scale varies between .79 and .95. In the present study, internal consistency reliability of the scale score as measured by Cronbach’s alpha was between .70 and .85.
Child abuse. An abbreviated 11-item version of the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 1994) was used to assess Child Physical and Emotional Abuse (CPEA) and Child Sexual Abuse (CSA) prior to 16 years of age. The CPEA subscale included five items, and the CSA subscale included six items, and items were answered on a 5-point scale (never true=0 to always true=4). Previous studies support the structural composition of the CTQ and its internal reliability (Bernstein et al., 1994). In this study, internal reliabilities for the CPEA (α=.74) and CSA (α=.84) subscales were adequate and good, respectively.
Sexual behavior. Participants were asked about condom use during the last four sexual acts.
STIs. Participants responded to a complete checklist of STIs, indicating whether, and with which, they had been infected. The presence vs. absence of STIs was used as a dependent variable.
Analyses
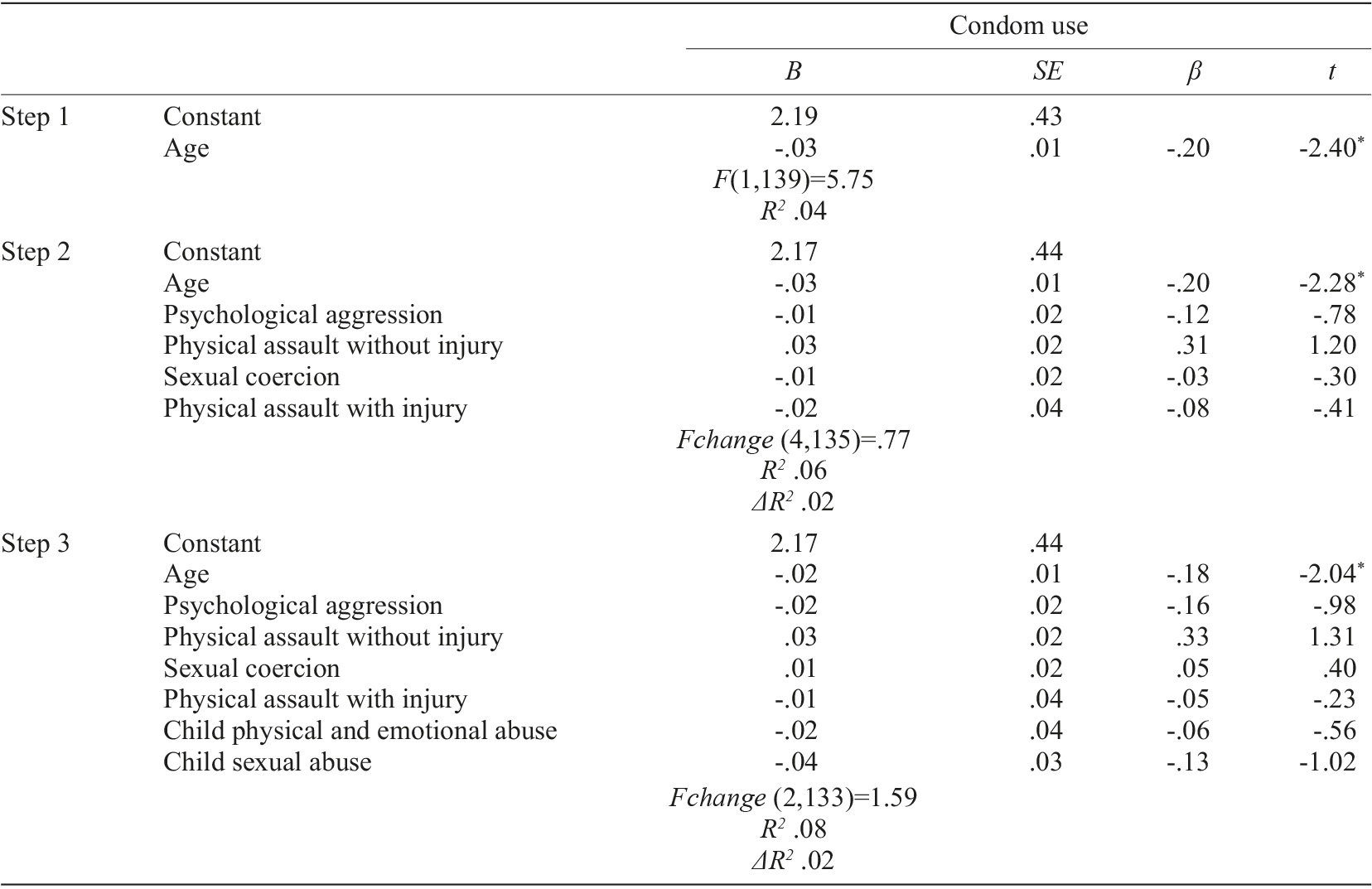
Descriptive analyses of demographic, clinical, psychosocial, and behavioral variables were performed. Mean and standard deviation were used to describe continuous variables. Categorical variables were described as absolute frequencies and relative frequencies. Furthermore, t-tests (for continuous variables) and Chi-square tests (for categorical variables) were conducted to compare demographic variables of women with and without IPV. Independent t-tests were used to establish differences in child abuse (CPEA and CSA), and condom use between women reporting IPV versus those who did not. Additionally, the Chi-Square test was used to find differences in the presence/history of STIs between female victims and non-victims of IPV. In order to analyze the association between the different types of IPV, childhood trauma, condom use, and presence/history of STIs, Pearson’s r Correlation coefficients were computed. Hierarchical regression analyses were performed to test the effects of different types of IPV and childhood trauma in predicting condom use. All analyses controlled demographic variables that were significantly correlated with condom use [age: r(141)=-.199, p<.05]. In the first step, age was included as covariate, followed by different types of IPV in step 2, and CPEA and CSA in step 3. This three-steps strategy allowed us to test the contribution of each group of variables while controlling the socio-demographic variables. For our current models the VIF values were all well below 10 and the tolerance statistics all well above 0.2; therefore, we can safely conclude that there is no collinearity within our data (Field, 2009). Terms were considered significant if the F value for the change in R 2 associated with each step was significant at p<.05. Hierarchical logistic regression analyzes were performed to test the impact of different types of IPV, CPEA, and CSA on the presence/history of STIs. The different types of IPV were included in step 1 and, CPEA and CSA in step 2. EXP (B), 95% confidence intervals (CIs) and p values are presented in each analysis. All analysis was performed with SPSS for Mac OSX version 23 software (SPSS, Inc., Chicago, IL).
Results
Demographics
The study sample consisted of 141 women, 61 (43.3%) victims of IPV and 80 non-victims (56.7%). The participants’ average age for women in violent relationships was 41.25 (SD=12.390) and 33.79 (SD=12.843) for women in non-violent relationships. Regarding education level, most women in violent relationships were high school graduate (29.5%), had some high school (26.2%), and are college graduate (24.6%), while those in non-violent relationships are mostly college graduate (55%). Most of the women (in violent and in non-violent relationships) were employed (59% and 57.5%, respectively). However, there is a higher percentage of unemployment among the women victims of IPV (34.4% versus 13.8%). In what concerns marital status, most women victims of IPV were married (31.1%) or divorced (23%), while those who were not victims were mostly single (51.2%) or married (30%). Most women victims of IPV had one or more children (77%) and the majority of non-victims had no children (55%). There were significant differences between women in non-violent and violent relationships regarding age, education level, professional status, marital status, and number of children, with women victims of IPV being older, having significantly lower education level, higher unemployment status, married, cohabitating or being divorced, and having more children than women that were non-victims.
Most of the victims were married to the aggressor (n=20; 32.8%) or were divorced (n=14; 23%). In fact, the majority of the victims were living with the perpetrator of the abuse (n=40; 65.6%). Almost all the victims were beaten first by the partner (96.7%).
Trauma and sexual behavior
Regarding intimate partner violence, most women victims and non-victims of IPV reported greater psychological aggression (n=93; 66%), followed by physical assault without injury (n=81; 57.4%), sexual coercion (n=81; 57.4%), and physical assault with injury (n=40; 28.4%). As for childhood trauma, most women reported greater physical and emotional abuse in childhood (n=99; 70.2%) than child sexual abuse (n=51; 36.2%). Regarding HIV risk behaviors, the majority of female victims and non-victims of IPV did not use a condom in the last four sexual acts (n=90; 63.8%). In fact, condom use in the last four sexual acts was used less than half of the times (M=1.22; SD=1.73). Regarding STIs, a possible health outcome of sexual risk behavior, 8.5% (n=12) reported having had a STI during their lifetime, namely hepatitis B (n=1; 0.7%), genital herpes (n=4; 2.8%), chlamydia (n=9; 6.4%), and pubic lice (n=1; 0.7%).
Differences between women with versus without IPV
Women reporting IPV reported more child physical, emotional, and sexual abuse (M=5.69, SE=6.04; M=4.51, SE=9.53) than did women not reporting such abuse (M=3.34, SE=4.01; M=.79, SE=2.04), a difference that was significant (t=-2.63, p<.05; t=-3.00, p<.05). Women who reported having suffered IPV reported also on average less condom use (M=.98, SE=1.63) than did those not reporting IPV (M=1.40, SE=1.79), a difference that was not significant (t=1.44, p=.152) (Table 1). Finally, women who reported IPV also reported more STIs than did women not reporting such abuse (n=9 versus n=3) and this difference was significant (χ 2 (1)=5.382, p=.020).
Relation between IPV, childhood trauma, and HIV risk behaviors
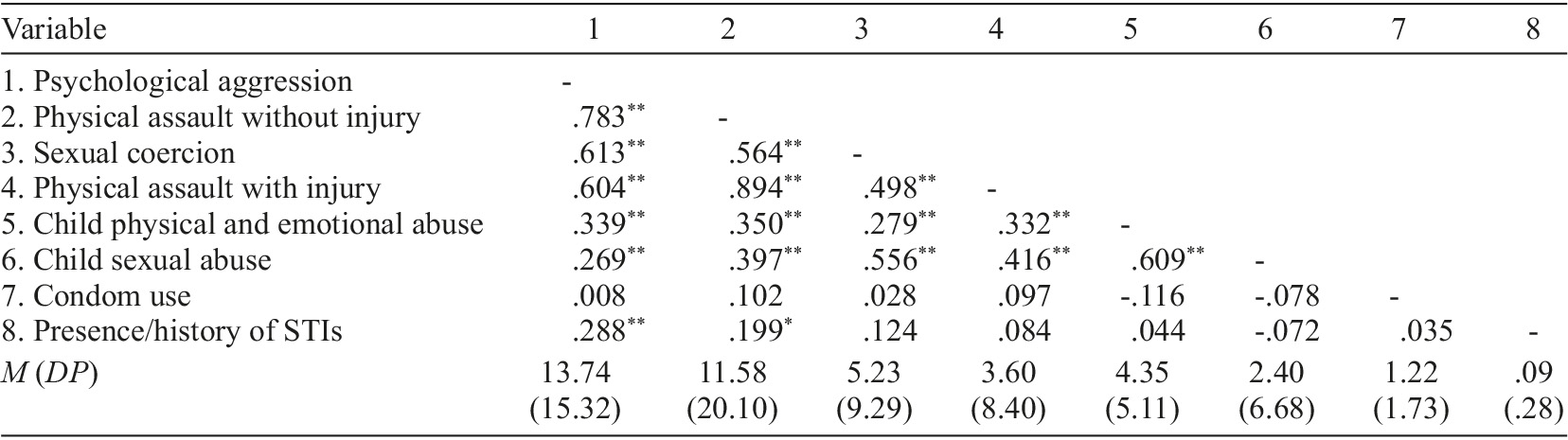
Correlations across the entire sample reveal that all dimensions of IPV were found to have positive significant correlations with childhood trauma. STIs history had also positive significant correlations with psychological aggression and with physical assault without injury. However, condom use did not reveal any significant correlations (Table 2).
Effects of IPV and child abuse on HIV risk behaviors
Hierarchical regression analyses were performed using the entire sample. For condom use, model 1, with the covariates as predictors (e.g., age), explained 4% of variance and was significant [F(1,139)=5.75, p<.05]. Model 2, in which IPV dimensions were added, explained more variance [R 2 change=.02, Fchange(4,135)=.77, p>.05]. As shown in Table 3, IPV dimensions accounted for an additional 2% of the variance in condom use after controlling for age but it was not significant. Model 3, in which child physical and emotional abuse, and child sexual abuse were added, explained a little more variance but this increase was not significant [R 2 change=.02, Fchange(2,133)=1.59, p>.05]. The total proportion of variance explained in condom use, explained by all the independent variables was 8%. In sum, being younger was the most important predictor of condom use in this sample (Table 3).
Table 3 The impact of IPV and child abuse on STIs
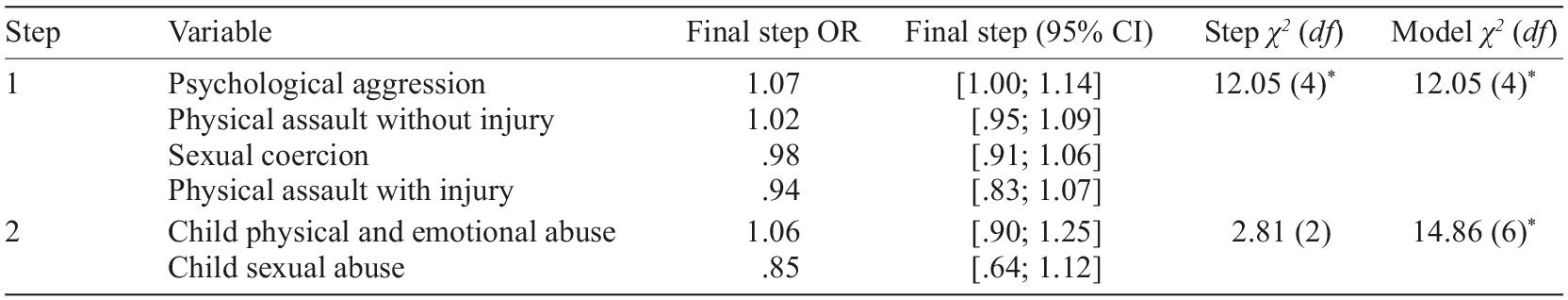
Note. OR=odds ratio. CI=confidence interval. * p<.05.
The logistic regression equation examined the ability of our model to predict presence/absence of STIs. Step 1 revealed significant effects of IPV variables, namely that women reporting psychological aggression and physical assault without injury were 1 time more likely to report STIs than women reporting no such abuse, and added significant amount of prediction to the null model, as the Nagelkerke R 2 of this step was .186 (see Table 3). Step 2 revealed no effects of childhood traumatic experiences. However, the inclusion of the second block of predictors allowed us to account for a significant amount of additional variance compared with both the null model and the first block model (Nagelkerke R 2 =.227). A test with all significant univariate correlates against a constant-only model was significant, χ 2 (6, N=141)=14.861, p<.05, suggesting that the correlates, as a set, distinguished reliably between those who reported STIs and those who did not. The Hosmer-Lemeshow test of goodness of fit was not significant, χ 2 (7, N=141)=3.992, p=.781, suggesting an adjustment fit to the data. Overall, the full model correctly classified 91.5% of the participants, compared with the 91.5% correctly classified by the constant-only model. The full model explained less than half of the variance in reported STIs (Nagelkerke R 2 =.227).
Discussion
The aim of this study was to assess the impact of IPV and childhood trauma on HIV risk behaviors. Additionally, other goal was to analyze the differences between victims and non-victims of IPV in terms of childhood trauma, condom use, and history of STIs.
In the present study, we found that women victims of IPV reported more physical, emotional, and sexual abuse in childhood than women who were not victims. The results of the present investigation are congruent with the study conducted by Kim (2017), who found that victims of IPV, compared to non-victims, experienced higher rates of childhood victimization, particularly physical and sexual abuse.
In what concerns condom use, the results indicated that, although there were no statistically significant differences between women victims and non-victims of IPV, victims showed less use of this contraceptive and protection method against STIs. These results are supported by the literature, which states that women who are victims of IPV are less likely to negotiate safer sexual practices and more likely to report more negative attitudes towards condom use than women who are not victims of IPV (Porter & Mittal, 2020), being more likely to engage in unprotected sex and, consequently, are at greater risk of acquiring STIs (Orchowski et al., 2020).
Regarding the history of STIs, women victims of IPV had more STIs compared to non-victims, a result supported by other studies that concluded that there is a statistically significant association between IPV and HIV infection (Li et al., 2014), and a significant association between experiencing any type of IPV and having had STIs (Nguyen et al., 2017).
The results of the present study also indicate significant positive relationships between the different dimensions of IPV and the dimensions of childhood trauma. These data are consistent with several studies (Costa et al., 2019; Pereira et al., 2020). For example, in the study by Costa et al. (2019) women who reported being abused during childhood also reported having experienced more rape in adulthood than women who did not report any child abuse. In addition, Pereira et al. (2020) also found that women tend to become victims when they experience violence in childhood.
As for HIV risk behaviors, namely condom use, the results obtained in the present study do not show a statistically significant relationship with IPV and childhood trauma. These results are not consistent with the literature review. For example, the study of Maxwell et al. (2015) indicated that the experience of women victims of IPV was associated with a lower probability of using contraceptives and a lower probability of using condoms. Likewise, Orchowski et al. (2020) showed that women engaged in unprotected sex as a result of the use of 32 forms of resistance to condom use by their intimate partner (such as physical force, deception or other forms of coercion to avoid using condoms during sexual intercourse), thus, the non-use of condoms is associated with physical, psychological and sexual victimization. Additionally, several studies state that people who have suffered an episode of sexual abuse in childhood have inconsistent condom use (Senn et al., 2017).
Regarding the history of STIs, the results of the present study show statistically significant and positive correlations with psychological aggression and physical abuse without injury. In fact, Saxena et al. (2019) analyzed the association between IPV and HIV, and found that women with HIV were more likely to report more severe forms of psychological violence and severe physical violence. Women who experienced severe forms of IPV were 3.5 times more likely to be HIV positive compared to those who did not experience severe IPV, indicating significant associations between severe forms of IPV and the presence of HIV among women. There are several explanations for this vulnerability, as there is evidence linking women’s experience of IPV and increased risk of STIs (Saxena et al., 2019). Several risk factors have been associated with IPV, which increase the likelihood of acquiring and transmitting HIV and other STIs, such as forced sexual activity, injuries to the vagina or other parts of the body, microscopic lacerations and tears in the anal and oral mucosa, as well as nail lesions on the skin and other sensitive areas, thus increasing the contact of the virus with the wounds, and in turn, increasing rates of transmission (Gilbert et al., 2016). Other risk factors that increase the probability of acquiring HIV and others STIs among women who are victims of IPV are the low negotiation of condom use or safer sex practices with sexual partners, the increase in risky sexual behaviors, and the fact that men that perpetuate violence are more likely to have multiple sexual partners and less likely to consistently use condoms (Porter & Mittal, 2020).
Adjusting for socio demographic factors, there was no evidence pointing that IPV contributed to inconsistent condom use. We would have expected that IPV would contribute to lower condom use. According to the study of Kusunoki et al. (2018), women who experienced physical IPV in their current relationship were less likely to use contraceptives; condom use was lower among women who, in their current relationships, had experienced physical IPV in the past; and women who experienced physical IPV used condoms less consistently. In addition, we also found that childhood trauma, although negatively associated with condom use, was not significantly associated with condom use in the regression model. However, several studies show that people who were victims of childhood sexual abuse have an inconsistent use of condoms (Senn et al., 2017).
Our results confirm some impact of IPV on the presence/history of STIs. Other studies also report a significant relationship between IPV and STIs. For example, Sigbeku et al. (2015) concluded that IPV predicts STIs, demonstrating that women who experienced any form of IPV were more likely to report STIs than non-victimized women, physical and sexual IPV experience was significantly associated with a history of STIs, and experiencing two or more types of IPV was significantly associated with a history of STIs. Also, certain types of IPV are more strongly associated with HIV risk behaviors. The literature suggests that men who use physical and sexual aggression in their relationships have more STI risk compared to men who don’t use violence because they have higher numbers of sexual partners, and exposure to high-risk partners and STIs. As a consequence, these men then place their primary romantic partners at higher risk through forced intercourse, inconsistent condom use, and partner concurrency (Casey et al., 2016).
However, childhood trauma was not associated with the presence/history of STIs in our study. This result is not supported by the existing literature, since women who are victims of childhood sexual abuse constitute a population that is at high risk of STIs, and there is, therefore, a need to work with these women in order to reduce the risk of STIs, namely HIV (Senn et al., 2017).
The results of the present study have important implications for clinical practice with women victims of IPV and for public health. The findings highlight the necessity of intervention programs addressing both intimate partner violence and childhood trauma to reduce HIV risk behaviors. Assessing childhood trauma and IPV should be included in routine primary care settings in order to prevent further abuse through the psychological treatment of trauma. Additionally, public health programs to prevent STIs should target victims of childhood trauma and IPV to promote safer sex negotiation skills. Also, considering the increased vulnerability of women victims, it is important to develop and implement psychological intervention programs, based on the Duluth Model (“power and control wheel”) and the model of social learning theory or sociocognitive theory (SCT). The Duluth Model, developed within the scope of Domestic Abuse Intervention Programs (Burge et al., 2016), has as main objective to make the aggressor not defend authoritarian relationships and achieve behaviors that allude to the “wheel of equality”, which promotes a more egalitarian attitude towards relationships, thus re-educating abusive men and their beliefs about IPV, women, namely their intimate partners, and gender stereotypes, basing themselves on feminist concepts and sociocultural ones of domination and control (Pence & Paymar, 1993). In addition to being an educational model, it also integrates cognitive-behavioral techniques, outlining how men use male privilege, emotional and economic abuse, violence, intimidation and isolation to control women, as well as coercion, denial, and use of children, and it is designed to protect survivors of domestic violence, while holding perpetrators accountable (Burge et al., 2016; Pence & Paymar, 1993). Likewhise, SCT emphasizes that new behaviors are learned through imitation of the behavior of others or through direct experience (Bandura, 1977), having as main principles, self-efficacy, that is, the belief in the ability to perform a required behavior (such as using condoms with an intimate partner), and expected outcomes, i.e., beliefs about outcomes, such as the belief that using a condom correctly will prevent HIV. Programs built on the SCT integrate information and attitude change to achieve motivation and the reinforcement of risk reduction and self-efficacy skills, in particular, the activities focus on the experience that people have talking with their partners about sex and condom use, positive and negative beliefs about condom use, and the type of environmental barriers they face towards risk reduction.
In this perspective, SCT highlights the use of behavior modeling to increase effectiveness in carrying out desirable behaviors and strengthen people’s cognition about risk and desirable goals by acquiring the behaviors necessary to achieve these goals, alluding to women’s awareness of their effectiveness in these behaviors (Bandura, 1997). Therefore, the results obtained in the present study show that Portuguese women victims of violence should be targeted with psychological intervention programs that are effective in reducing sexual risk behaviors, in order to acquire skills of self-efficacy and sexual assertiveness.
As with any research, the present study has some important limitations. The sample consists of women from victim support associations and primary health care services only in northern Portugal, which may not be representative of the broader population. Additionally, the reliance on self-report measures, particularly for sensitive issues like IPV and childhood trauma, can lead to biased responses due to social desirability or recall bias. Finally, the fact that this study is a cross-sectional study is another limitation, as it is not possible to establish the temporality between IPV in female victims and HIV risk behaviors. Future research should address these limitations by including a broader population and biological markers of STIs in a longitudinal study.
Despite the limitations, the results of the present study allow us to better understand the relationships between IPV, childhood trauma and HIV risk behaviors in a sample of Portuguese women. The results show the relevance of IPV and childhood trauma in HIV risk behaviors, so it is essential to intervene in this population, through interventions that are based on reducing risky sexual behaviors. It is crucial that health units carry out frequent screenings, in order to identify cases of IPV in women, developing prevention and intervention programs that consider violence prevention and the development of skills to negotiate consistent condom use to reduce the risk of STIs, namely HIV, and promote regular HIV testing. It is also crucial to develop intervention programs with children who are victims of childhood abuse, in order to reduce the consequences in their lives and prevent them from becoming victims of IPV in adulthood, as well as to reduce future risk behaviors for HIV and other STIs. In conclusion, this study shows the impact of IPV on physical and sexual health and highlights the need for effective interventions to promote support, self-efficacy, assertiveness, and protection in sexual behavior among female survivors.